Home
Rheumatoid Arthritis and Juvenile Idiopathic Arthritis

Rheumatoid arthritis (RA)
Health and economic impact
Rheumatoid arthritis (RA) is a chronic condition with a significant impact on individuals and society. It leads to musculoskeletal problems, reduced physical function, and affects overall quality of life. RA also imposes a substantial economic burden due to healthcare costs and decreased work capacity. RA can lead to various complications and comorbidities, including cardiovascular disease and lung problems. However, modern treatment approaches have significantly improved outcomes and reduced associated risks.
Understanding RA: diagnosis and risk factors
Early diagnosis and prompt treatment initiation are crucial to managing RA effectively. Modern genetic research has revealed insights into the genetic factors underlying RA, including the influence of specific genetic markers like the HLA system. Additionally, environmental factors such as smoking, infections, alterations in the gut microbiome and socioeconomic status play a role in RA development. Understanding these factors could lead to improved prevention and treatment strategies.
Future prospects in RA treatment
Assessment of disease activity is essential for monitoring RA progression and guiding treatment decisions. Treatment strategies focus on reducing inflammation and preventing joint damage, with the goal of achieving remission or low disease activity.
Despite significant advancements in RA treatment, challenges remain, including predicting treatment responses and addressing therapeutic failures. Research efforts continue to explore new therapeutic targets and develop more effective treatments for RA.
In summary, RA is a complex disease influenced by genetic and environmental factors. Early diagnosis, targeted treatment, and ongoing monitoring are essential for managing RA and improving outcomes for affected individuals.
Juvenile Idiopathic Arthritis (JIA)
A chronic autoimmune disease in children
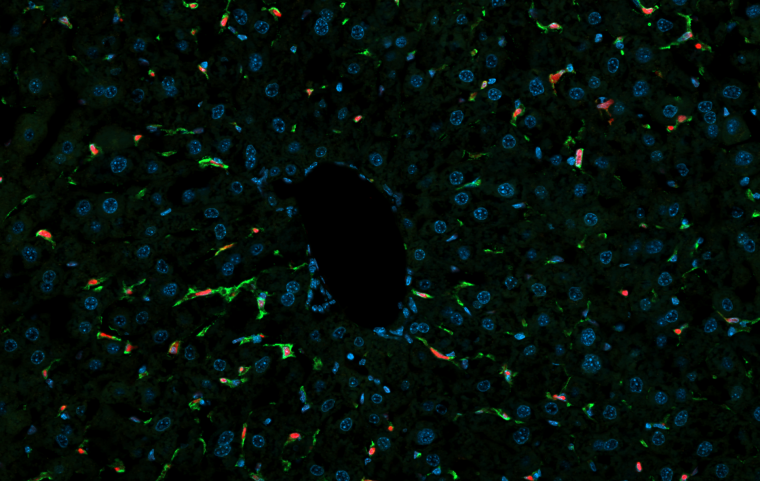
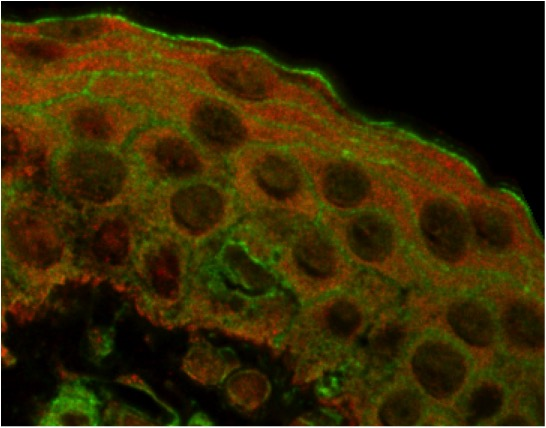
Juvenile Idiopathic Arthritis (JIA) is a chronic autoimmune disease primarily affecting children under 16 years old. This condition involves inflammation of the joints, leading to stiffness, swelling, and pain, which can impair daily activities and quality of life. Its exact cause remains unclear, but genetic and environmental factors likely contribute. JIA comprises several subtypes, each with distinct symptoms and prognoses that most likely correspond to different diseases classified under the same terminology of JIA by simplicity. Among these different clinical subsets, systemic JIA (also known as Still’s disease) occurs in 10% of cases and is characterized by a variety of inflammatory multiorgan manifestations in addition to arthritis. In addition, some of these patients develop a hyperinflammatory state termed macrophage activation syndrome which is considered as a severe complication associated with significant mortality. Similar clinical manifestations as in systemic JIA can also occur in adults (adult-onset Still’s disease).
Managing JIA: treatment and research
JIA treatment aims to alleviate symptoms, reduce inflammation, and preserve joint function through medications, physical therapy, and lifestyle modifications. These novel therapies can also control the severity of systemic manifestations.
Although advanced treatments have improved clinical outcomes, a significant number of patients remain unresponsive to treatment, highlighting the need to better understand disease progression and remission to support patient stratification in treatment pathways.