Limiting energy in neurons exacerbates epilepsy
A team led by UNIGE and EPFL has made a counterintuitive discovery in mice: epileptic seizures are more violent when the energy-producing pathway in their neurons is blocked.
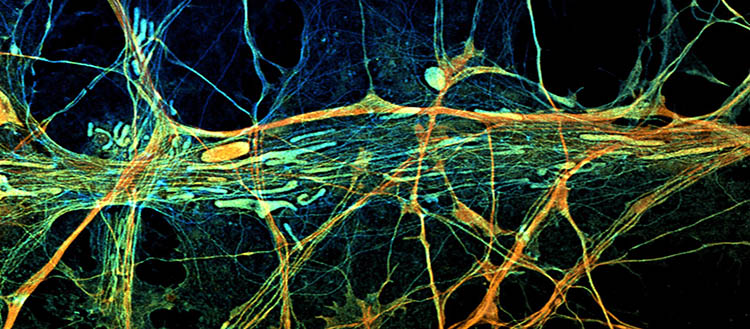
Mitochondria (tubular structures) within the cytoskeleton filaments of neurons observed by fluorescence microscopy. (c) Marine Laporte
Epilepsy, one of the most common neurological disorders, is characterized by the spontaneous repetition of seizures caused by the hyperactivity of a group of neurons in the brain. Could we therefore reduce neuronal hyperactivity, and treat epilepsy, by reducing the amount of energy supplied to neurons and necessary for their proper functioning? This was tested by a team led by scientists from the University of Geneva (UNIGE) and the EPFL. The researchers discovered that, in mice, the seizures were actually exacerbated. They observed that a reduction in the amount of energy led to an increase in the level of calcium in neurons, making them hyperexcitable. These dysfunctions could be corrected when mice were fed a ketogenic diet, which is rich in lipids and has been used since antiquity. This work is published in the journal eLife.
Our brain, which represents only 2% of our body weight, consumes more than 20% of the sugar we ingest. This considerable need for sugar provides the energy necessary for the function of the billions of neurons responsible for the emission and propagation of nervous messages, via electrical signals. This conversion of sugar, and more precisely of glucose, into energy is carried out by the mitochondria, small intracellular organelles considered as the «energy factories» of the cell.
The key role of the cell’s «energy factories»
The laboratory of Jean-Claude Martinou, professor in the Department of Molecular and Cellular Biology at the Faculty of Science, is interested in how mitochondria work. His group had already discovered the universal carrier that allows pyruvate, a product of glucose catabolism, to enter into mitochondria. He is now investigating the role of the mitochondrial pyruvate carrier (MPC) in neuronal activity and whether a defect in the transport of pyruvate in mitochondria could be linked to certain neurological diseases, notably epilepsy.
Epileptic seizures are the manifestation of cerebral hyperactivity resulting from hyperexcitation of neurons, often in the cerebral cortex. «It seemed interesting to us to test whether suppression of the mitochondrial pyruvate carrier, and thus the decrease in the amount of energy supplied by the mitochondria, could reduce neuronal hyperexcitability occurring during epileptic seizures», explains Jean-Claude Martinou, last author of the study.
Mice lacking the MPC are prone to epileptic seizures
The biologists administered a pro-epileptic drug, capable of inducing epileptic seizures, to normal mice and to mice whose cortical neurons lacked the MPC. In normal mice, injection of a low dose of the drug did not induce seizures. On the other hand, and contrary to the initial hypothesis, in mice lacking the MPC, very severe, even fatal, seizures occurred as soon as low doses of the pro-epileptic drug were administered.
Upon further analysis of what was happening in these neurons, the biologists found that the neurons without MPC had abnormally high levels of calcium, a crucial element for the proper transmission of nerve messages. «Pyruvate imported into mitochondria not only plays the role of a fuel for the cell, but it also allows mitochondria to sequester calcium. It turns out that it is this second function that is involved in the triggering of epileptic seizures. Since it is no longer trapped by the mitochondria, the calcium remains free in neurons and its concentration increases, which makes the neurons hyperexcitable,» explains Carmen Sandi, professor at EPFL and coauthor of the study.
The secrets of the ketogenic diet
Since ancient times, patients suffering from epilepsy have found that a ketogenic diet, rich in fats and low in carbohydrates, allows them to avoid seizures. Ketone bodies, produced during a ketogenic diet or fasting, are produced by the breakdown of lipids in the liver. They are imported into the brain for which they represent an essential energy source, especially during a fast. They can enter mitochondria without the need of carriers and are used to provide energy.
«We found that MPC-deficient mice fed on a ketogenic diet or treated with ketone bodies had much less severe seizures. With this diet, the functions of mitochondria and neurons are restored, and the calcium level is normal,» said Marine Laporte, researcher in the Department of Molecular and Cellular Biology and co-first author of the study. This work, financed by the Swiss National Science Foundation and the Kristian Gerhard Jebsen Foundation, helps to explain the epileptic seizures frequently observed in patients with mitochondrial pathologies as well as to consider a treatment based on ketone bodies, less drastic than ketogenic diets.
24 Mar 2022