Replicating patients’ tumours to test different treatments
UNIGE Researchers have developed in vitro tumour models that incorporate components of the tumour and elements of the patient’s immune system to test the effectiveness of treatments.
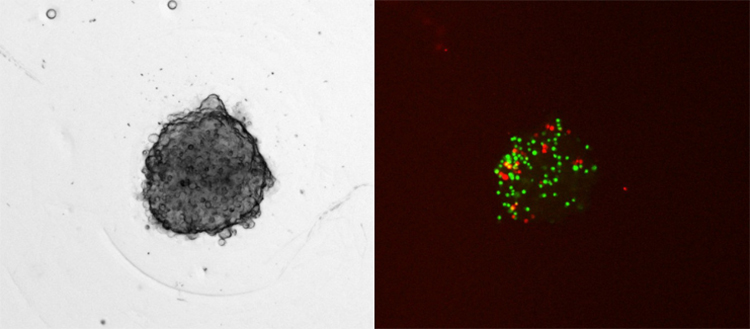
The spheroid includes cancer cells, endothelial cells, fibroblasts, monocytes and human T cells. Fluorescently labelled immune cells (green, monocytes; red, T cells) can infiltrate the preformed spheroid within 12 hours. Scale bar = 100 µm. © Magdalena Rausch
Every tumour is different, every patient is different. So how do we know which treatment will work best for the patient and eradicate the cancer? In order to offer a personalised treatment that best suits the case being treated, a team of scientists led by the University of Geneva (UNIGE), Switzerland, had already developed a spheroidal reproduction of tumours that integrates the tumour cells, but also their microenvironment. However, the immune system had not yet been taken into account, even though it can either be strengthened or destroyed by the treatment given to the patient. Today, the Geneva team has succeeded in integrating two types of immune cells that come directly from the patient into the spheroidal structure, making it possible to test the various possible treatments and select the most effective. These results can be read in the journal Cancers.
In order to test cancer treatments, scientists use 2D cultures of cancer cells. However, these are only an artificial system, as they do not represent the 3D tumour in all its complexity. This is why the team of Patrycja Nowak-Sliwinska, professor at the Section of Pharmaceutical Sciences of the Faculty of Science of the UNIGE, has developed a spheroidal structure that reproduces the microenvironment of the tumour. “The idea is to create a 3D structure from the cells of the tumour, while also integrating the fibroblasts – cells that make up the mass of the tumour – and the endothelial cells, which allow the tumour to feed and be vascularised.” This method, which has since been used by the University Hospitals of Geneva (HUG), allows us to get closer to the tumour as it is present in the patient’s body. “However, an important factor was still missing: the cells of the immune system”, explains the Geneva researcher.
The critical role of the immune system in the fight against cancer
The immune system is the primary fighter against tumours and it reacts differently depending on the treatment prescribed to the patient: its effectiveness can either be increased or decreased. Today, the Geneva team, in collaboration with the universities of Lausanne and Amsterdam, has succeeded in integrating two types of immune cells into its spheroidal structure: macrophages and T lymphocytes. “This technological advance makes it possible to test the effects of a treatment not only on the tumour, but also on the immune system!”, enthuses Magdalena Rausch, researcher at the UNIGE’s Section of Pharmaceutical Sciences and first author of the study. To do this, the scientists first take cells from the patient’s tumour to recreate it in vitro in the form of a spheroidal structure, and then they isolate the immune cells and inject them into the 3D structure. “Once this step has been completed, which takes 24 hours, we can test the various possible treatments for this cancer on our reproduction of the tumour and study which one will be most suitable for the patient, taking into account the effects on the tumour cells, but also on the immune system”, explains Patrycja Nowak-Sliwinska.
This technique, which is relatively inexpensive and fast, would make it possible to propose a personalised treatment for each patient, while offering an effective alternative to several animal experimentations. “This platform opens up many possibilities for testing drug combinations, taking into account the different types of cancer, their mutations and the immune reactions specific to each person treated”, concludes Patrycja Nowak-Sliwinska.
